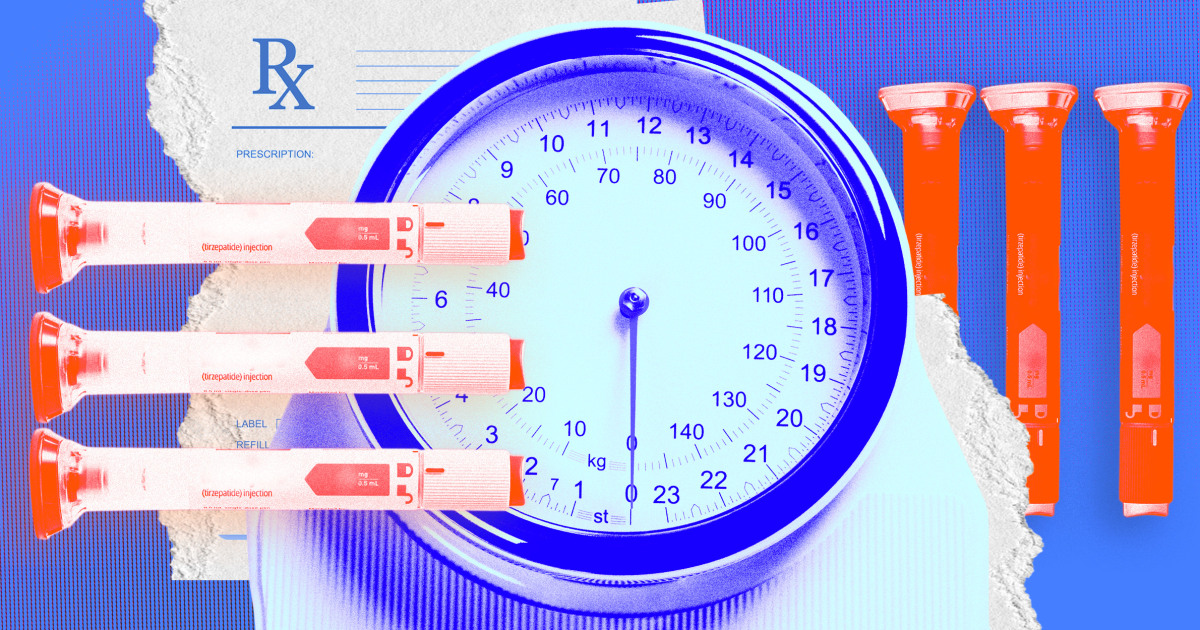
If an Eli Lilly weight-loss drug is approved, it could become the best-selling drug of all time, but concerns are growing over who will be able to afford it.
Experts are confident that the drug, called tirzepatide, will receive approval from the Food and Drug Administration sometime next year. If that’s the case, it would join two other popular, and expensive, recently approved weight-loss drugs on the market, Wegovy and Saxenda, both from drugmaker Novo Nordisk.
Annual sales of tirzepatide could reach a record $48 billion, according to an estimate by Bank of America analyst Geoff Meacham. Another Wall Street analyst, UBS’s Colin Bristow, estimated the drug would reach $25 billion in annual sales, a number that would still surpass the record of $20.7 billion set by AbbVie’s rheumatoid arthritis drug Humira in 2021. .
Kelly Smith, a spokeswoman for Eli Lilly, declined to comment on the cost of tirzepatide. Outside experts said the drugmaker may be able to price it similar to Wegovy, which has a list price of about $1,500 for a month’s supply, and Saxenda, which cost about $1,350 for a month’s supply.
If the FDA confirms the drug’s efficacy, a “fair” price for tirzepatide could be around $13,000 a year, or about $1,100 a month, said Dr. David Rind, medical director of the Institute for Clinical and Economic Review, a research group that helps determine fair prices for drugs.
The drugs have been shown in clinical trials to be highly effective for weight loss. All three drugs, which are given by injection, work in a similar way: They are a class of drugs called GLP-1 agonists, which mimic a hormone that helps reduce food intake and appetite.
However, Eli Lilly’s tirzepatide also mimics a second hormone, called GIP, which in addition to reducing appetite, can also improve the way the body breaks down sugar and fat.
A phase 3 clinical trial found that a high dose of tirzepatide helped patients lose an average of 22.5% of their body weight, or about 52 pounds, better than any drug currently on the market. The more patients in the trial had a body mass index, or BMI, of 30 or more. In trials, Wegovy and Saxenda reduced body weight by about 15% Y about 5%respectively.
Are weight loss medications covered by insurance?
At lower doses, all three drugs are already approved to treat diabetes.
- Tirzepatide is sold under the name Mounjaro for diabetes.
- Semaglutide, when marketed for weight loss, is sold in a higher dosage and is called Wegovy; at a lower dose, it is marketed for diabetes and sold as Ozempic.
- Similarly, a higher dose of the drug liraglutide is sold under the name Saxenda for weight loss, and a lower dose is sold as Victoza, for diabetes.
With the exception of Mounjaro, which was approved earlier this year, versions of the drugs used to treat diabetes are covered by most insurers.
That is not always the case when they are prescribed for obesity.
Obesity carries a unique stigma, said Dr. W. Scott Butsch, director of obesity medicine at the Cleveland Clinic’s Bariatric and Metabolic Institute. Many doctors, he said, still see it as a behavioral problem rather than a medical one.
That belief, plus the fact that older anti-obesity drugs aren’t very effective, has made insurers reluctant to cover many newer therapies, he said.
“You have a bias,” Butsch said, adding that insurance companies ask for more proof of the benefits of obesity drugs than they normally would for other types of drugs.
Some insurers can select one of the weight-loss drugs and offer coverage, he said, but often restrict access to only patients who meet a certain threshold, such as a BMI greater than 30.
What’s more, Butsch said, not everyone responds the same way to a weight-loss drug. If the drug covered by insurance isn’t effective for that patient, there are usually no other drug options left, he said.
Dr. Holly Lofton, director of the weight management program at NYU Langone Health, regularly prescribes the new drugs to her patients, but many, she says, are denied coverage by their insurance. “Patients tell me that it seems to them that insurance companies want to wait until they are so sick that they need a drug the most,” she said.
Lofton said some of his patients will end up spending thousands of dollars out-of-pocket on drugs for a few months while they negotiate with their insurer for coverage. His insurance plan typically doesn’t reimburse patients for money they’ve already spent on drugs, he added.
Dr. Fatima Stanford, a specialist in obesity medicine and director of equity in the division of endocrinology at Massachusetts General Hospital in Boston, said private insurance coverage for obesity drugs is patchy, with treatments often restricted to the most expensive plans.
Medicare does not cover them. Anti-obesity drugs are not a mandatory Medicaid benefit, although some states have chosen to include them, he said.
Obesity is considered a chronic disease., And like any other chronic disease, most patients are expected to take the drug for their entire lives, a huge financial burden if forced to pay out-of-pocket, Stanford said.
The only people likely to be able to afford a drug like tirzepatide on their own, he said, will be the “very rich.”
Despite access barriers, the UBS Bristow analyst said he still expected tirzepatide to be a blockbuster drug for obesity, noting that the US. we are already seeing supply shortages for drug as injection for diabetes.
“It’s pretty clear how strong the demand is,” he said.
What do you need to change?
Lofton, of NYU Langone Health, said coverage for obesity drugs may not improve until more people in the medical field change their view of obesity. It’s not something that diet, exercise, or sheer willpower can fix; instead, it’s a dysregulation of fat cells in the body, he said.
Bias and stigma around obesity are rampant in the medical community.
It’s “evident in all healthcare professionals, including doctors, nurses, dietitians and others,” said Lisa Howley, an educational psychologist and senior director of strategic initiatives and partnerships for the Association of American Medical Colleges.
A review posted last year in the research journal Obesity found that health professionals have implicit and/or explicit weight-biased attitudes toward people with obesity.
But changing the minds of the medical community, and with it, the insurance companies, is extremely difficult. Requiring obesity drugs to be covered by insurance may require legislative action, Stanford said.
In 2021, House lawmakers introduced The Obesity Treatment and Reduction Act, which would have allowed the federal government to expand Medicare Part D coverage to include anti-obesity drugs. The legislation had 154 bipartisan cosponsors, according to congress.govbut did not receive a vote on the House floor before the term ended.
America’s Health Insurance Plans, or AHIP, a trade group representing insurance companies, declined to say whether it would support coverage of tirzepatide should the drug gain FDA approval next year or other anti-obesity drugs.
“Health insurance providers routinely review the evidence for drugs and surgical treatments for obesity, offering many options to patients, ranging from lifestyle changes and nutritional counseling to surgical interventions and prescription drugs,” David said. Allen, AHIP spokesperson.
Butsch, of the Cleveland Clinic, said he’s hopeful insurance companies will cover tirzepatide.
“We are really seeing highly effective anti-obesity drugs for the first time,” he said. “The benefit is real.”